By Dr. Donna S. Barsky, R.Ph, D.Ph
This short guide can help you manage a discussion with your doctor about your vascular health. This is an important issue that can affect your health.
What is cholesterol? Cholesterol is a fatty, wax-like substance found in the cells of your body and blood. It comes from your diet and is also produced by the body. Total cholesterol in the blood includes various components including HDL, LDL, and triglycerides. Cholesterol has an important role in the overall healthy functioning of the body. The body needs the right level of cholesterol to function properly, but too high levels of cholesterol increase the risk of cardiovascular disease.
Hypercholesterolemia is the medical term for high cholesterol. High cholesterol is a significant risk factor for coronary heart disease, peripheral arterial disease (PAD), and stroke.
High-density lipoprotein (HDL) is known as the “good” cholesterol because it is believed to have protective properties against heart attack. Some medical experts believe there are two major roles of HDL. One, it carries cholesterol away from the blood vessels and back to the liver so the liver can eliminate it from the body. Two, HDL removes the excess buildup of cholesterol from arterial plaque. If you have a low HDL on your blood test (<40 mg/dl), you will not have the benefit of HDL’s cardiac-protective properties. Exercise, weight loss and addition of nicotinic acid derivatives can help to increase these levels.
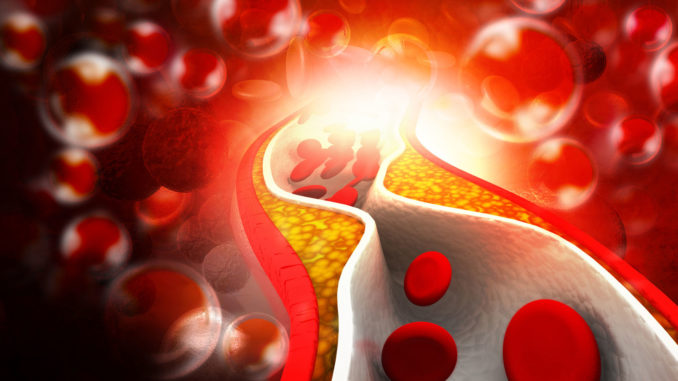
Atherosclerotic or artery plaques are mostly made up of cholesterol and calcium. These plaques deposit on the inside wall of the artery. The buildup of plaque can reduce blood flow and eventually a complete blockage can occur, either from the plaque itself or due to rupture of the plaque, with collection of a blood clot on top of the plaque. Depending on the blood vessels involved, this process can cause a stroke, heart attack, or PAD. If PAD occurs during this process, it can result in decreased function or loss of function in other organs of the body, or an arm or leg.
Low-density lipoprotein (LDL) is known as the “bad” cholesterol because it plays a role in the development of atherosclerotic plaques. Think of LDL as butter floating in the bloodstream. High LDL levels are the main target of cholesterol-lowering therapies and lifestyle changes. If you have a high LDL on your blood test (>100 mg/dl), it will increase your risk for coronary heart disease, vascular disease, and stroke. Current guidelines recommend lowering LDL more aggressively in patients with more risk factors or known atherosclerotic plaque.
Triglyceride is a form of fat made in the body. There are various factors that can cause high levels of triglyceride, including obesity, diabetes, decreased physical activity, cigarette smoking, and excess consumption of alcohol and trans fat.
The importance of routine cholesterol screening is that it can identify high-risk individuals. Early treatment of these individuals can decrease the incidence of coronary heart disease, stroke, and PAD. The US Preventive Services Task Force (USPSTF) strongly recommends that men aged 35 years and older, and women aged 45 years and older have their cholesterol tested to screen for lipid disorders. According to the USPSTF, there is good evidence that cholesterol testing can find asymptomatic individuals at risk for heart disease, stroke, or vascular disease, and early treatment of these high-risk individuals can prevent and decrease their risk of cardiovascular disease.
The USPSTF also recommends that younger adults (men aged 20 to 35 and women aged 20 to 45) have their cholesterol tested to screen for lipid disorders if they have other risk factors for coronary heart disease. These other risk factors include diabetes, a family history of cardiovascular disease before age 50 years in male relatives or age 60 years in female relatives, a family history of familial hyperlipidemia, and multiple cardiovascular risk factors including obesity, hypertension, and tobacco use. The early treatment of these higher-risk individuals can prevent cardiovascular disease.
Currently, the USPSTF has no recommendation for or against routine cholesterol testing in younger adults (men aged 20 to 35 or women aged 20 to 45) in the absence of known risk factors for cardiovascular disease. The USPSTF found good evidence that cholesterol testing in low-risk young adults can detect some individuals at increased long-term risk of cardiovascular disease, but the absolute reduction in risk as a result of early treatment in most individuals is small before middle age.
Treatment options include both lifestyle changes and drug therapy. Lifestyle changes include dietary counseling to understand the benefits of a diet low in saturated fat and high in fruits and vegetables, regular exercise, stopping tobacco use, and maintaining a healthy weight. Drug therapy can be more effective than any other treatment option alone and these include nicotinic acid derivatives (niacin, Niaspan), bile acid sequestrants (Cholestid, Questran), cholesterol absorption inhibitors (Zetia), Omega-3 esters (Lovaza, Omega-3 Oils), fibrates (ie, fenofibrate, Gemfibrozil), and statins (Lopressor, Zocor, etc). New research data suggests that statin therapy may lead to regression in atherosclerotic plaque, and more studies are being conducted to confirm this finding. All statins should always be taken at bedtime because that is when most cholesterol is produced by our systems. In most people, a combination of many therapies can give great results and decrease risk substantially.
If you have any concerns or questions about your risks, be sure to ask your doctor or call the pharmacy for recommendations. TexasStar Pharmacy can be reached at 972-519-8475.



